According to published figures, chronic insomnia affects millions of adults around the world, and it is a multifactorial disorder with far-reaching consequences for mental and physical health. This huge book on insomnia attempts to provide an overview of the subject and discuss the science behind it, its medical implications, the immediate and long-term effects, and ways of coping with it. The authors feel they can help the chronic insomniac understand this troubling condition, access healing since time immemorial, and improve their general quality of life.
 Introduction
IntroductionInsomnia is defined as trouble either falling asleep or staying asleep, and it can impair every dimension of life. While occasional sleeplessness can be considered a normal occurrence, chronic insomnia tends to prevail, become worse, and make one ill if left unchecked. We have laid down the biology of sleep and insomnia, the implications of insomnia on health, and some practical means of alleviating its symptoms in the short and long run.
Sleep is a biological necessity with complex processes to restore mental and physical functions. Neurologically, sleep is subdivided into stages of non-rapid eye movement sleep- NREM sleep (stages 1-3) and rapid eye movement sleep (REM sleep). The architecture of sleep is tightly regulated by circadian rhythms and homeostatic sleep drives.
Circadian rhythm is the internal regulatory system-that tells you when to sleep and wakes time-and affects many bodily functions. The regulation of these rhythms depends on light cues from the external environment captured by the suprachiasmatic nucleus (SCN) located in the hypothalamus. Such disturbances could lead to insomnia but are most notable in shift workers or people with jet lag.
The homeostatic drive for sleep is said to increase sleepiness directly depending on the length of time spent awake. Accumulation of the neurochemical adenosine in the brain is a major contributor to this homeostatic drive for sleep. Caffeine blocks the action of adenosine, and certain medicines might ramp things up further, obstructing the sleep cycle.
The duration of disturbance in sleep initiation, sleep maintenance, and nonrestorative sleep persists for at least three times per week for three months or longer. Chronic insomnia, being long-term, is a disorder that requires complex therapeutic intervention, as opposed to acute insomnia, which is a short-term event usually preceded by a temporary event or stressor.
Chronic insomnia is characterized by persistent difficulty initiating or maintaining sleep, or experiencing non-restorative sleep, for at least three nights per week over a period of three months or longer. Unlike acute insomnia, which is often linked to temporary events or stressors, chronic insomnia is a long-term condition that may require comprehensive therapeutic interventions.
The etiology of chronic insomnia can be multifactorial, involving a combination of genetic, psychological, and environmental factors. Neurobiological research reveals that dysregulation in neurotransmitters such as serotonin, dopamine, gamma-aminobutyric acid (GABA), and orexin can contribute to sleep disturbances.
There can be significant disruptions in day-to-day performance and well-being by even short-term sleep disturbances. It is crucial to comprehend the immediate effects so that instant adjustments in lifestyle and therapy can be made.
Sleep deprivation disturbs memory, decision-making, and concentration. Emotionally, one tends to feel a bit cranky, with rising anxiety and mood fluctuations. The instantaneous modulation of sleep disruption and emotional dysregulation calls for immediate intervention in individuals facing acute sleep disturbances.
Short-term insomnia can lead to a certain level of fatigue and impair motor coordination. With fatigue comes a chance for increased accidents. The stressor of bad-quality sleep can induce a chain reaction of endocrinal activities that further raise cortisol levels and impede metabolism.
Sleep deprivation reduces productivity. Employees with poor sleep quality may feel less efficient, commit more errors, and find their working relationships strained, all of which in turn increase stress contributing to the already burdening state of insomnia.
 Long-Term Health Impacts of Chronic Insomnia
Long-Term Health Impacts of Chronic InsomniaChronic insomnia is, in a way, a long-term risk to health, and beyond short-term problems, a lot of health casts in jeopardy. Extensive scientific research has shown a strong link to chronic insomnia and certain serious health conditions:
Sleep disruption, beyond a certain duration, will contribute to the development and aggravation of a whole range of mental disorders. Their incidence is higher in patients with chronic insomnia than in controls. Neuroimaging studies have demonstrated alterations in specific brain regions linked to mood regulation, such as the prefrontal cortex and limbic system.
It has been established that chronic insomnia correlates with cardiovascular disease; this correlation is made via the following gradually-extending mechanisms: inflammation; autonomic dysregulation; persistent elevated blood pressure. Sleep is restorative for the cardiovascular system; chronic insomnia can become the basis for cardiovascular pathologies.
Chronic sleep deprivation has long been considered a major player in metabolic unrest, say in increased chances of obesity and type 2 diabetes. Poor sleep affects the body’s capacity to handle insulin and glucose; it also suppresses the immune system, thus leaving people vulnerable to infections.
With long-term insomnia come neurodegenerative changes. Research has shown that not getting enough sleep may speed up the ingraining of cognitive decline with age, thus helping in processes like Alzheimer’s, where cleaning activity against neurotoxic proteins such as beta-amyloid is impaired.
A comprehensive assessment of the patient’s medical, psychological, and sleep history makes up the diagnostic process for insomnia. There are various methods and assessments employed by clinicians to diagnose the condition with accuracy.
A sleep diary can offer useful clinical information on sleeping behavior, sleep duration, and possible factors that may precipitate insomnia episodes. Self-reported data give much-needed information to recognize patterns and rate the severity of sleep issues.
Polysomnography is a sleep study performed for evaluating brain waves and oxygen levels, heart rate, and breathing during sleep: Very helpful to differentiate sleep disorders and co-morbid conditions like sleep apnea that might lead to insomnia.
An actigraphy sensor is worn on the wrist to quantify movement and activity and the data is obtained for more than a few weeks. This non-invasive method may support the sleep diaries and assist in the identification of deviations in sleep behavior.
Chronic insomnia is treated generally from a multi-pronged angle. Medical treatment tackles the biological factors instigating disturbances in sleep, whereas psychological therapies (CBT) try to alleviate the thoughts and behaviors that further worsen the state of insomnia.
Medications can be short-term and effective for relieving the symptoms of insomnia. The commonly prescribed include:
CBT-I is regarded as the gold standard for treating chronic insomnia. It consists of the following components:
Scientific studies have demonstrated that cognitive behavioral therapy for insomnia involves long-lasting changes at minimal risk of side effects, making this an excellent therapy for long-term management.
Lifestyle modification forms a vital part of insomnia management. Changing daily activities and the sleep environment often significantly improves sleep quality.
Sleep and wake on a schedule, even on weekends. Keeps your body clock steady. Ideally, adults should sleep for approximately 7-9 hours per night.
The sleep environment is vital for sleep quality. These include:
Eating large amounts at bedtime slows the process of normal falling asleep, as does caffeine or nicotine in the hours preceding sleep. Limit caffeine, nicotine, and large meals in the hours before sleep to help support the natural sleep cycle.
Mindfulness, progressive muscle relaxation, and deep-breathing exercises give relief from anxiety and stress and help improve sleep quality. They can be merged into a better CBT-I strategy.
Insomnia is mostly a symptom or an aggravating condition of various other psychological or medical problems. Thus, it is important to treat these underlying conditions to relieve sleep disturbances.
People suffering from psychiatric disorders such as depression, anxiety disorders, or post-traumatic stress disorder (PTSD) most often have sleep deprivation. Management of the primary disorder is usually alongside behavioral intervention so as to address resultant sleep disturbance.
Chronic pain, respiratory problems such as asthma or chronic obstructive pulmonary disease (COPD), and gastrointestinal disorders can interfere with one’s sleep. Multidisciplinary treatment approaches targeting these conditions may provide relief from insomnia symptoms.
Sleep medicine will continue evolving. There is ongoing research into newer treatment modalities and technologies for the management of insomnia. Several promising areas include:
The condition of patients with insomnia has been greatly improved with respect to access to care for such patients as mobile applications and Internet-based CBT-I programs have been shown to be effective in other conditions. These platforms also boast interactive modules and sleep tracking with real-time feedback, making custom-designed therapy applicable.
Studies in neuromodulation such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) are exploring how these techniques could be used for modulation of brain activity related to sleep regulation. Although at very initial clinical trial application, the results have been promising for refractory insomnia.
New advances in genomics and neuroimaging make room for personal approaches to insomnia’s treatment. With genetic profiling and sleep-related biomarkers combined with lifestyle data, a treatment could be tailored to the patient’s specific needs, thus achieving the best effects in treatment use.
There are many practical things one can do immediately to improve his sleep from night to night for acute insomniacs.
Some types of food contribute to good sleep:
Acute stress can be dealt with relaxation techniques through deep breathing and visualization exercises, for example.
Mindfulness meditation, guided imagery, or listening to calm music before bed can reduce the mental clutter that often keeps one awake.
Chronic insomnia often requires prolonged efforts to change lifestyle behaviors. Several evidence-based techniques can be recommended to achieve long-term sustainable improvements in sleep:
Regular Exercise Quite often, moderate exercise should be done, at least some several times during a week, to make sleep more sound. However, the exercise must be completed at least some hours before bed to avoid hasty heartbeats at the time of trying to fall asleep.
Since chronic insomnia is really an interplay with mental health, it may cause a need for long-term therapy, counseling, or support groups for success. In such cases, professional assistance may be required to overcome those associated symptoms of anxiety or depression that have caused sleep deprivation.
Sleep diary or keeping records on sleep from a wearable can help to inform the subject about the success of the strategies implemented. It can then be further fine-tuned, over time, with personal sleep data in developing individualized treatment plans.
It is critical to consult healthcare professionals who specialize in sleep medicine in all aspects of treatment when dealing with chronic insomnia. Most evaluations determine the occasions to change therapy or medication based on altered symptoms.
Coping with insomnia can also be achieved using other complementary paradigms aside from regular treatment.
Yoga and tai chi are forms of exercise that are beneficial for sleep, more than reducing physiological arousal and levels of stress.
Acupuncture has relevance in insomnia as a complementary treatment modality, but clinical studies have also suggested possible modulation of neurotransmitter release, thereby improving sleep quality. However, such treatment protocols need to be standardized.
Some individuals may benefit from the utilization of dietary supplements, such as melatonin, magnesium, or valerian root, but take caution using these under professional supervision, as they may interact adversely with other medications.
Overall, chronic insomnia is a multifactorial disorder affecting almost all aspects of health and daily life. Individuals can learn to deal well with insomnia by understanding the biological and neurological bases of insomnia, along with short-term and long-term consequences to health. Sustainable management of such a problem could be achieved by multitargeting medical treatment, behavioral interventions, lifestyle modifications, and newer emerging therapies.
An integrative approach to immediate treatments and long-term strategies will work best for improving sleep and quality of life in adults with chronic insomnia. It is imperative to partner with health practitioners in developing a customized approach that combines conventional and complementary therapies. In many cases, with sincere effort and wise decision-making, restful nights can once again be reclaimed and enjoyed, along with improved overall health.
Aside from this extensive scientific and practical overview, we strongly advise those suffering from i[ersistent insomnia to seek advice from specialists. The research, however, does not cease here. It evolves with time and is promising towards more specific therapeutic options in the future.
For those interested in exploring the scientific research behind insomnia, the following sources provide further detailed information:
The information contained in this guide is meant for educational purposes and should not replace individualized medical advice. Please consult a healthcare provider for personalized suggestions tailored to your specific situation.
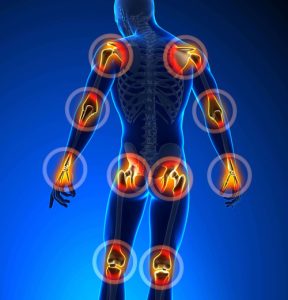
Joint pain is a health complaint from which millions of people across the globe suffer. It can develop in people of any age and when it’s there for some time can lead to drastic discomfort and a reduced quality of life. This resource is an extensive overspill on the causes, symptoms, diagnosis, treatment as well as prevention of joint pain. Backed by scientific research, evidence from acknowledged medical authorities, and clinical studies, this article acts as a great guide to understanding joint pain and management strategies. Whether your joints only pain occasionally or you are suffering from chronic joint pain, this guide is here to prepare you with all kinds of in-depth, reliable information and insights.
 Introduction
IntroductionJoint pain, or arthralgia as it is often called even in medical circles, may be caused by an acute injury or a chronic disease. Diagnosing the cause of joint pain is critical for its effective treatment given how complex this symptom can be. Joint pain can often be more than a fleeting discomfort, for instance, it may denote the existence of systemic or general diseases such as rheumatoid arthritis and osteoarthritis or even infection. Thus it is significant to recognize the biomechanics of joints, state their inflammatory processes, and identify one’s lifestyle factors when studying joint pain.
In this resource, we delve into:
Joint pain can arise from a multitude of underlying conditions. A proper diagnosis allows for treatment to be targeted exactly where it is needed. Some causes include the major ones such as listed below:
OA is one of the most common causes due to which older people deal with joint pain. Progressive degeneration of the cartilage cushion at the ends of bones occurs with age. This means that the bones will rub off each other and create pain, swelling, and reduction in movement. Clinical studies, including ones summarized by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), have proven that significant factors that enhance susceptibility include joint overuse, obesity, and hereditary predisposition.
Rheumatoid arthritis is an autoimmune disorder in which the immune system of the body mistakenly attacks the joint tissues. In this case, the joint lining undergoes inflammation, which causes a huge level of pain and damage to the tissues. Research published by the American College of Rheumatology further highlighted the insight into the chronic inflammatory process of rheumatoid arthritis, making early diagnosis and treatment important in order to avoid joint destruction.
Gout is a specific form of arthritis due to the deposition of uric acid crystals in joints. Therefore, acute episodes of gout in patients are characterized by intense pain, redness, and swelling. Dietary triggers include the ingestion of purine-rich foods (e.g., red meat, seafood) and alcohol. The mainstay of management incorporates lifestyle modifications and medications to lower urate levels.
Infectious arthritis is the term used to describe a situation when bacteria, viruses, or fungi invade and infect a joint. Bacterial arthritis is the most common type of arthritis and, if not treated brutally fast, may inflict lots of damage to the joint. The common bacteria responsible are Staphylococcus aureus and Streptococcus species. Prompt diagnosis is essential, as the rapid course of these infections may leave the only option for treatment being drainage and the administration of antibiotics.
Beyond rheumatoid arthritis, other autoimmune diseases such as lupus (systemic lupus erythematosus) may give rise to joint pain symptoms. In systemic lupus, the systemic inflammation is affecting multiple organs, including joints. A wealth of studies has been conducted supporting the use of immunosuppressive medications in aiding autoimmune-induced joint pain.
Joint injuries from accidents, falls, or sports-related incidents can present with acute joint pain. Any trauma may be spraining the ligaments, tearing the meniscus, or fracturing. Untreated injuries may evolve into chronic conditions over the years that predispose the affected individual to eventually suffer from osteoarthritis later in life.
Contingent factors such as obesity, a sedentary lifestyle, and poor biomechanical alignment may aggravate joint pain. Increased body weight augments the stress on joints like the knees and hips, contributing greatly to degenerative changes. Joint pain usually attributes to repetitive strain injuries and bad postures.
The symptoms of joint pain can differ widely based on the underlying cause. However, common signs and symptoms include:
Recognizing these symptoms is crucial in foreseeing the possible onset of joint problems. However, since many of these symptoms may overlap in different conditions, a thorough medical examination by a professional becomes paramount.
 Diagnosis
DiagnosisFor a proper diagnosis of joint pain, a complete evaluation of the patient’s history will be taken and a physical examination will be conducted, followed by a series of diagnostic tests. Here are the following entailments that may form the diagnostic procedures:
A medical professional will take a thorough medical history, including information about duration, severity, and pattern of the pain. The history also includes questions about previous injuries, family history of joint diseases, and any observable triggers. The physical examination assesses the tenderness, swelling, and motion of the joints, which helps narrow down the likely causes.
Imaging is of crucial importance in the diagnosis of joint disorders. Some of the most common imaging techniques include:
Many studies published in radiology journals show that imaging modalities have drastically improved the ability to diagnose joint conditions early and thus improve treatment outcomes.
Patients may undergo blood tests and fluid analyses to look for markers of inflammation, infection, or autoimmunity. Tests may include:
The information gained from laboratory tests is essential for distinguishing the forms of arthritis that exist, allowing proper direction of therapy.
The treatment of joint pain is generally complex and involves so many variables; types of patients presenting with different etiologies and symptomatology require different treatments. This interplay of diverse factors translates into treatment strategies that aim to minimize pain, restore function, and prevent additional joint harm. The following sections provide an overview of pharmacological whereas non-pharmacological treatment measures will follow thereafter.
The very first treatment option for relief of joint pain is medication. The type of medications includes:
Physical therapy has a vital place in joint pain treatment. Tailored exercise programs facilitate joint mobility, muscle strengthening around the joint, and overall reduction in discomfort. The common modalities include:
Research from rehabilitation and sports medicine advocates that adherence to an exercise program will reduce joint pain and even slow down the disease progression in degenerative joint diseases.
Some remedies are often used in conjunction with orthodox treatments for joint pain relief. These include:
For sudden debilitating joint pain that does not respond to conservative management, surgical options may come into play. These include:
The decision to operate is usually made on a per-patient basis, depending on the patient’s age, overall health status, and which joint is involved.
Although not all cases of joint pain can be prevented, lifestyle changes and immediate attention can drastically minimize risk factors and slow down the evolution of joint-related disorders.
Maintaining a healthy weight is crucial to reducing the load on weight-bearing joints like knees and hips. Studies prove that even a small percentage of weight loss can be associated with a significant reduction in joint pain and increase joint function. The weight management scheme comprises a balanced diet paired with exercise.
Regular exercise not only helps in weight maintenance but also helps with joint mobility and muscle strengthening. Low-impact activities such as swimming, cycling, and yoga may be particularly helpful for those at risk of developing joint pain. Consultation with a healthcare provider or physical therapist in creating a personal exercise plan is necessary.
The application of joint protection methods to everyday activities can minimize injury risk. Examples include the following:
The earlier you evaluate joint pains, the easier they are to manage. Being on the lookout for early signs of joint problems and seeking timely medical attention may keep minor problems from evolving into chronic problems. Regular consultations with your health care provider, especially among individuals with a family history of joint diseases, may lead to early diagnosis and intervention.
While joint inflammation is one of the first signs when something goes wrong, a wholesome load of omega-3 fatty acid-rich foods, as well as vitamin D and C, antioxidants, etc., indicate that these compounds might be useful in reducing the inflammatory process and improve function at the level of joints. Emerging evidence and literature are corroborating the role of nutrition in the management of inflammatory processes resulting from causes like arthritis and other joint disorders. Looking up the services of a nutrition advisor or dietitian can help when one wants to create a personal diet to address their needs.
The information provided herein is strongly backed with scientific evidence and clinical research. For instance, several longitudinal studies have signified the contribution of chronic inflammatory state in the pathogenesis of osteoarthritis and rheumatoid arthritis. The research published in esteem journals like The Journal of Rheumatology and Arthritis & Rheumatism dwelt much on the molecular drivers of joint degeneration, together with the efficacy of various treatment modalities.
Furthermore, recent trials have shown that patients suffering from joint pain exhibit beneficial outcomes as a result of a multimodal approach which integrates pharmacotherapeutic, physical therapy modalities, and lifestyle change. Medical bodies like the American College of Rheumatology are quasi-perpetual in continuously updating guidelines on recommendations to make them reflective of new evidence.
Joint pain cannot really be cured. It needs a lifestyle that would be preventive, and that involves taking measures more than just relieving pain. Some of the practical advice includes the following:
Joint pain manifests in various forms and it can significantly restrain its victim’s capacity to function in day-to-day life and, thus, his or her quality of life if not properly managed. By knowing various causes ranging from osteoarthritis and other degenerative diseases to autoimmune conditions like rheumatoid arthritis, and knowing the many symptoms, people will have better chances understanding the very complicated diagnoses and treatment techniques.
Management of joint pain through a concerted approach of combining the traditional medicine with specialized therapies, daily changes, and surgery when required. Indeed, the advances in medical science continue to add credence to what these authorities like NIAMS and the American College of Rheumatology recommend; they truly insist on early treatment and personalized treatment regimens.
Those who are considering options for treatment or looking forward to take preventive measures must certainly collaborate with healthcare providers. With the right-informed approach, many people with joint pain will stand to significant improvement, recover mobility, and thus great quality of life.
While this offers all the detail regarding joint pain and treatment, it is not intended as a replacement for a medical opinion. If symptoms persist or worsen over time, consult with a healthcare provider for an individualized evaluation and treatment plan.
For comprehensive and more insightful studies and exploration into these topics, try the following resources:
Being proactive and most importantly informed about joint health is the first step toward managing joint pain effectively. With the best mix of treatment and prevention, any person can lead an active, post-injury life despite suffering from joint pain.
Migraine is an episodic headache that is often so painful that it renders the patient unable to continue with his normal functions. The headache is also associated with a combination of neurological and autonomic symptoms and gastrointestinal symptoms. This article reviews in detail the clinical presentation and diagnostic strategies as well as therapeutic options available for modern management of migraine on the basis of clinical practice and the new American Academy of Neurology (AAN) treatment guidelines. This would constitute an educational material for healthcare providers and patients who want to know more about this common condition.
 Clinical Presentation
Clinical PresentationMigraine usually manifests as a headache, which is often unilateral, moderate to very severe. Although the exact pathophysiology is extremely complex, certain observations drawn from clinical neuroimaging have revealed neuronal hyperexcitability, vascular dysregulatory process, and trigeminovascular system activation.
Symptoms of migraine can be highly individualistic; nevertheless, the following are common:
According to epidemiology, about 12 to 15 percent of the population suffers from migraine headaches. Women are about three times more likely than men to have generalized headaches. It occurs primarily from adolescence to early adulthood. The condition is known to impair the quality of life and productivity significantly. The guidelines of the American Academy of Neurology recognize individual differences in the form of varying symptomatology and call for a thoroughtaking of clinical history to clinch diagnosis.
It has now been shown, as a result of new approaches to investigation, that migraine should no longer be viewed as a vascular disease, but rather as the combination of vascular changes induced by neurogenic inflammation, as well as cortical spreading depression. The following is a diagram that demonstrates the understanding of the pathophysiological cascade in migraines today:
 Diagnosis
DiagnosisMigraine is clinically diagnosed primarily through the assessment of the patient history and symptomatology. Without a definitive laboratory test, however, various diagnostic criteria and tools help facilitate accurate and timely diagnosis to minimize risk misdiagnosis and ultimately aid proper management.
The International Classification of Headache Disorders (ICHD-3) and evidence-based guidelines define these criteria that are used for the diagnosis of migraine:
Differentiating migraine from other headache syndromes is paramount. One could include among many others the broad differentials:
Migraine is a clinical diagnosis; however, there may be a case for neuroimaging with MRI or CT for a patient with atypical presentation or with red-flag symptoms (for instance, neurologic deficits, sudden onset severe headache). AAN guidelines indicate that imaging is not done routinely on patients with a clear clinical history consistent with migraine unless:
To rule out systemic causes of headache, ancillary tests (e.g. blood work such as complete blood count, inflammatory markers) may be performed when clinically indicated.
Management of migraine may be comprehensive, acute, and prophylactic, lifestyle changes, and drug intervention for resistant cases. Treatment must be based on the levels of evidence and the clinical indications as defined by the current treatment guidelines in AAN.
Acute therapy is intended to relieve migraine attacks rapidly while minimizing associated symptoms and restoring functionality. The following treatments are stratified into evidence levels:
The main objective of preventive therapy is the reduction of the frequency, intensity, and duration of migraine episodes. AAN guidelines recommend offering preventive therapy to patients with:
Specific preventive regimens are classified according to the level of evidence and clinical indication, as follows.
In terms of a more comprehensive migraine management plan, non-pharmacologic interventions must be included:
There are additional difficulties in treating a chronic migraine (the occurrence of 15 or more headache days each month with at least 8 days fulfilling the criteria for a typical migraine) since a truly multidisciplinary approach involving both pharmacological and non-pharmacological measures would be necessary for patients whose headaches reject more simple treatment or classical definitions. In refractory cases:
Although generally benign, certain clinical situations encountered in migraine do require an immediate evaluation and intervention. Emergency signs include:
Complications that warrant urgent management include medication overuse headaches, status migrainosus (prolonged migraine lasting more than 72 hours), and side effects of non-opiate analgesics, sometimes resulting in medication-rebound headaches.
The management of migraine is patient centered and individualized according to expert consensus. Current treatment strategies thus continue to develop based on ongoing clinical trials and advances in pharmacology. Some key expert recommendations include:
Recent updates to the treatment guidelines of the American Academy of Neurology urge more use of CGRP-targeted therapies in patients suffering from chronic and refractory migraines as they showed robust clinical trial data and a better profile regarding tolerability compared to traditional agents.
The following stepwise clinical approach can be applied in the evaluation and management of migraine:
The perspective on the pathway to heal this disorder requires an all-encompassing and holistic individualized treatment approach. Such perplexing clinical manifestations, coupled with potential considerable functional impairment, necessitate compliance with the clear standards of evidence-based diagnosis and management offered by the AAN. Good management of a migraine requires prompt intervention with patient education, proper fellowship, and collaboration among many professionals aimed at developing an individualized treatment strategy, beginning with the recognition of the unique symptoms of a migraine and differentiating those from other headache disorders before treatment can begin-with abortive and preventative therapies included.
Expert opinion states that combining pharmacologic agents with lifestyle modifications and behavioral therapy optimally influences clinical outcomes and improves suffering individuals’ quality of life. Health care providers must remain current on emerging treatment approaches and changing AAN guidelines to remain in step with the latest directions.
Research in the future is expected to further clarify migraine neurobiology, refine diagnostic biomarkers, and widen the spectrum of targeted therapies available for treating the condition. For now, treating migraines relies on expert judgment, patient-centered planning for therapy, and application of the established guidelines.
References: The American Academy of Neurology guidelines, ICHD-3, alongside more recent peer-reviewed journals on neurology and headache medicine.
For additional insights and audiovisual content, healthcare providers and patients are encouraged to refer to the following:
Clinical Notes denotes the need for continuous research and education in migraine management. By fusing evidence-based care with individualized patient management, health care providers can have a major impact on this condition and its outcome for millions of people around the world.
They will then continue to put together a story for an ever-growing group of patients affected by migraine, made more acute with each step in the current evolution of the understanding of migraine from neurobiology through treatment.
Ultimately, integrating a robust clinical history with targeted physical examination and judicious use of diagnostic modalities forms the bedrock of effective migraine management. Evidence-based treatment strategies, as advocated by the American Academy of Neurology, support the judicious use of both abortive and preventive therapies that are tailored to individual patient profiles, ensuring that each treatment plan is as unique as the patient it aims to serve.
 Clinical depression is really a medical condition fully changing the life style of the individual victims in the entire world. Generally, it may be challenging to confirm and consequently manage the disease due to its dimension. This article will discuss the symptoms and signs of clinical depression in more detail; explain the way how to diagnose depression; look at available therapeutic methods recommended by various clinical guidelines, which are based on the most recent evidence and admissible literature; and support those who are willing to seek help for depression by availing available sources. This content is written for the benefit of any adult person who has an interest in the subject and has a need for information, but it is also recognized that the emotional concepts this article touches upon, could be particularly fit fully for a certain group of people who are in distress. Therefore, it is essential to require an approach to a health care professional, especially supported in an official manner of diagnosing and prescribing medication.
Clinical depression is really a medical condition fully changing the life style of the individual victims in the entire world. Generally, it may be challenging to confirm and consequently manage the disease due to its dimension. This article will discuss the symptoms and signs of clinical depression in more detail; explain the way how to diagnose depression; look at available therapeutic methods recommended by various clinical guidelines, which are based on the most recent evidence and admissible literature; and support those who are willing to seek help for depression by availing available sources. This content is written for the benefit of any adult person who has an interest in the subject and has a need for information, but it is also recognized that the emotional concepts this article touches upon, could be particularly fit fully for a certain group of people who are in distress. Therefore, it is essential to require an approach to a health care professional, especially supported in an official manner of diagnosing and prescribing medication.
For most people, the word clinical depression often referred to simply as depression does not mean being a little sad or feeling bad over anything. It is a complex condition with various symptoms that can be mild in some persons and severe to others. There is little difference on the prevalence of mental health disorders, but a reversal happens on the way the society relates to mental health – as seen from today’s generation. There is a difference in the manner that depression – and the situation is vast – has been approached and how it impacts on human lives today. As shown by data derived from the most recent published works from scientifically respected sources like research papers and health magazines, depression has been progressively intruding on peoples lives with progression intensifying even more in view of the current modes of living.
Emotions are affected: People diagnosed with clinical depression mostly stay in a state of sorrow, lacking hope or feeling empty most times. The emotional symptoms of the disorder have made them lose interest in whatever they loved doing most of the time. The scourge of feelings of going down the drain and being worthless will smear them with too much guilt and pessimism concerning the future. Quite recent studies have shown figures that virtually one in six people will experience such emotional problems at some time or other.
Cognitive Symptoms: One of the effects of depression is that it impairs cognitive functions. The deterioration could reach such a level that it could make a person have trouble concentrating and being indecisive and even to experience some slight memory loss. These could result in an inability of an individual to participate in most activities or to produce accordingly in a job set-up. Several studies have confirmed that cognitive functions associated with depression will be found afterward and not immediately during the acute phase, hence requiring early intervention.
Physical Symptoms: Apart from the emotional and cognitive domains, clinical depression also has different physical manifestations in appetite shield and weight changes. Sleep disturbances, including insomnia or frequent oversleeping, and persistent exhaustion are also observed in patients with depression. Pain, chronic fatigue syndrome, and gastrointestinal issues may be presented by these individuals. Just recently, one study pointed out that more than 50% of patients who were diagnosed with moderate to severe depression had reported at least one somatic symptom in addition to their usual dysthymic situation. This emphasizes the importance of the need for a comprehensive approach.
Behavioral Symptoms: Social withdrawal is a symptom that is relevant in diagnosing depression. There is a group of patients whose relationships severely suffer as well as their work or education life due to lack of motivation or power, when they are depressed. This imprisonment to oneself makes it worse for most patients who opt to be left alone. It is important that the family, friends, wife, husband, partners, children and parents of a depressed person recognize the change and try to encourage the patient to get treatment.
Understanding the symptoms is an act and process that always brings the desire for the depressed person to get a diagnosis and treatment for their depression. These symptoms usually manifest in the illness at its primary stages therefore facilitating an earlier intervention preventing further complications and ensuring faster medical recuperation.
In order to achieve a depression diagnosis that is credible, certain steps and procedures are conducted to eliminate any form of bias in that decision, these steps and procedures include specialty consultants or psychologists. The sentence ‘making a depression diagnosis’ should not however be overused, for this requires an overview of events contributing to the current and past health of a patient, as well as other comorbid disorders. Such guidebooks also make essential criteria for assessment of these patients using instruments such as categorical manuals like the Diagnostic and Statistical Manual of Mental disorders (DSM-5) in making a diagnosis.
Initial Phase: The diagnosis of depression typically begins with the first stage of the evaluation process. This covers in-depth questioning of the subject about their problems, their personal and medical history, and their recent adverse or shocking experiences that could have precipitated the onset of the illness. Healthcare practitioners may use standardized tests and assessment tools such as the Patient Health Questionnaire with a 9-item scale (PHQ-9), which, in some clinical trials, has been found to be a beneficial predictor of response.
Physical Examination: People are asking themselves does physical examination was conducted or certain physical illnesses, endocrine disorders, or medications can mimic or exacerbate symptoms of depression. The medical evaluation would therefore include some common laboratory tests.
The healthcare practitioner might order some simple blood tests such as thyroid function tests, vitamin levels, and tests for other metabolic conditions.
Psychiatric Assessment: Depression cannot be diagnosed without psychological evaluation. For this purpose, a mental health professional – this could include a psychiatrist or a psychologist – does an interview to investigate the character, intensity and period of the symptoms.
Besides this, they also investigate how these symptoms work out in the life of the individual? Are there any measures being taken to manage the depression at work or in a situation when they are required for a particular purpose? In this connection efforts are made not only to establish whether the clinical depression criteria are met but also to find the of the particular symptoms existence – social phobia and bipolar syndrome inclusive.
The Collaborative Diagnosis: In many medical cases, therapeutic protocols are used in which a combination of formulations is utilized. This might be that the primary care physician optimizes the pharmacological management of the patient or refers the patient to a counselor. More recent studies addressing the field of mental illness are beginning to show the clear positive benefits of an encompassing health service delivery system integrating again many components of the total health care system, and it is indeed proving to work well in depressed patients.
It is essential to acknowledge the fact that a determination of depression is not entirely defined. The approach is customized to avoid giving more than necessary diagnosis in different patients and considering how each is also affected with other associated psychological or even physical problems. Consulting informed professionals is necessary in order to make an accurate diagnosis and create a treatment plan which will serve its purpose.
On receiving a diagnosis, a person suffering from clinical depression has the option of several treatment modalities. The treatment plan remains very personalized, as it is understood that what works on an individual may not necessarily work on someone else. There are various avenues for depression help, including medications, psychotherapy, lifestyle changes, and holistic remedies.
Medication: Antidepressant medications are commonly included in the treatment of clinical depression. Antidepressants, particularly the group of drugs called selective serotonin reuptake inhibitors (SSRIs), are used to stabilize one’s mood by modulation of chemical balance in the brain associated with depression. Recent studies over the past five years have shown that when used together with psychotherapy, antidepressants are said to be most effective in patients with moderate or severe depression. Nevertheless, any form of prescription should consider the unique health profile of the patient and strict medical supervision in its administration.
Psychotherapy: Psychotherapy provides useful treatment methods for managing clinical depressive symptoms. Some major talk therapies used include cognitive behavioral therapy (CBT), interpersonal therapy (IPT), and dialectical behavior therapy (DBT). These therapies help clients to identify negative thought patterns they engage in and challenge them, develop constructive coping strategies, and work on interpersonal issues that may be contributing to the depression. Mental health professionals agree that psychotherapy provides not only tools to manage present symptoms, but also the building of skills to prevent relapse.
Holistic and Lifestyle Approaches: Holistic and lifestyle approaches for complementing treatment of depression are often recommended by several healthcare practitioners. Regular physical activity, healthy eating, and mindfulness practices such as meditative activities-all can help with mood enhancement and general mental well-being. Recent studies within the last 5 years have indicated that exercise, in particular, can be comparably as effective as medication in improving depressive symptoms by increasing the level of endorphins and enhancing sleep quality for some patients.
Combined Treatment Approaches: Combined Treatment Approaches: Combining medication and psychotherapy often brings about the most favorable treatment outcomes. Such an integrative approach greatly attends to both the biological and psychological facets of depression. Recent research provides evidence that patients being treated with both pharmaco- and psychotherapy show greater improvement than when treated with either modality alone.
Emerging Treatments: Emerging Treatments: Research in the field continues to open new avenues for treating clinical depression. Of note, Transcranial Magnetic Stimulation (TMS) and Ketamine infusions have emerged as candidates to either replace or supplement treatment in patients who do not respond to standard treatments. Although these treatments are still under investigation with regard to their long-term efficacy, early expert opinion would suggest they may be a promising treatment for depression that has failed to respond to other interventions.
It is imperative that anyone seeking depression help consult with healthcare providers to discuss the full range of treatment options and design a strategy that best fits their individual needs. Evidence-based research continues to evolve, offering hope to those affected by clinical depression and underscoring the importance of early and personalized treatment interventions.
 4. Seeking Mental Health Support and Resources for Depression Help
4. Seeking Mental Health Support and Resources for Depression HelpThere should be a nice support system for dealing with clinical depression. People who can offer mental health support include professionals, family members, friends, and community organizations. One important thing about depression is that it can make people feel isolated, knowing that help can exist with one’s struggle.
Building a Support Network: Clinical depression has the challenge in personal relationships and daily interactions. They should be opened up to trusted friends and family members regarding their struggle. A truly supportive relationship can provide emotional comfort and, as well.
Professional Resources: There are various resources in the world to access mental health support. Licensed mental health professionals such as psychologists, psychiatrists, and clinical social workers are specially trained to provide appropriate care in the form of counseling. Community mental health centers and local clinics usually have a sliding scale fee loaded in their programs, ensuring the money aspect is not a deterrent to treatment.
Online Resources and Hotlines: The internet has actually become one of the most valuable aids on helping seek depression healing. Well-known sites like the National Alliance on Mental Illness (NAMI), Mental Health America, and the Substance Abuse and Mental Health Services Administration (SAMHSA) feature relevant information about clinical depression, self-improvement strategies, and resources in the neighborhood. The National Suicide Prevention Lifeline, a national helpline available in many countries, provides round-the-clock assistance and guidance during critical times.
Support Groups: That’s a good idea if one connects with those who have been or are now in depression scenarios. Support groups-in-person and online-give chances for individuals to experience and share within a secure environment. In these groups, members will learn how others manage their symptoms, learn new coping strategies, and provide them with peer support in crises.
Innovative Community Programs: These include education, workshops, and group therapy sessions specific to mental health support available in some communities. Such programs have been proven to enhance global wellbeing and empower participants in managing their mental health.
It is really important to ask for help, however scary it might seem. If you think you or someone you know is suffering from clinical depression, it is worthwhile for the person to think seriously about seeking mental health assistance and getting professional help for their depression; it could change their life. Note that the information here is for educational purposes and does not provide any professional recommendations. It is hence important to contact a healthcare provider to get the correct diagnosis and treatment plan.
Over the five years, whatever studies have proved into the ways of clear insight into the clinical depression have, however, proven to strengthen the concept that depression is most treatable conditions requiring a multidisciplinary approach. Early detection followed by timely intervention is extremely important to minimize long-term impact of the disease, thus underscoring the experts in psychiatry and psychology.
“Early intervention by a combination of therapeutic and pharmacological methods has really proved to be very effective despite the fact that depression is a complicated and multi-dimensional phenomenon,” says India-born psychiatrist Dr. Emily Carson. “And more than ever before, our focus will be personalized care, which recognizes the uniqueness of a patient’s history and circumstances.” As they are, Dr. Carson’s views are backed up by evidence from many studies that revealed it was likely that recovery rates would increase when treatment plans for individualized patients rather than standardized forms of treatment would be used.
New large-scale mental health studies have indicated some very shocking figures, which compel the prioritization of mental health support. As for example, about one in 8-10 adults experience episodes degenerated to moderate and severe clinical depression at some point of the lifetime, according to a study held in 2021. Other studies show that only about 50% people depressed get remedied, which highlights a major lack of mental health support services in various communities.
Such research initiates the understanding between new treatment modalities- neurostimulation techniques and digital therapy platforms. These techniques are highly promising for patients where the traditional antidepressants failed to show adequate response. There is a general consensus among the experts that some of the innovations would help in decreasing the treatment resistance and enhancing the overall quality of life.
However, the advocacy has never ceased, and expert groups keep emphasizing the need to destigmatize mental health treatment. Their belief is that the language and social perceptions around clinical depression and treatment should change in judgment-reflecting it toward compassion, understanding, and evidence-based practice. Society can thus take critical leaps in progress delivering depression help, with delayed care missed and why it should be sane timely and effective for those in need.
The clinical depression is a composite one. It does not stop only at affecting the mood; it causes gross distortions in the cognitive and physical domains of almost all lifestyles. Diagnosing these symptoms-from a state of continuous sadness, having cognitive difficulties, to sometimes being changes in behavior-is the very first step toward getting an accurate depression diagnosis. As discussed, the complete evaluation most often required by health care practitioners includes a psychiatric assessment and, if relevant, also a physical examination to exclude underlying conditions.
They have different kinds of treatments like medications, psychotherapy, or changes in lifestyle, and many experts have started saying that there’s a combination that makes a treatment much more effective. Research has even been looking into newer methods like neurostimulation techniques and digital formats for managing mental health. The message is clear to the readers: legs in symptoms of any kind of depression, they should consult the healthcare providers for accurate diagnosis and personalized treatment options.
Hopefully, this article has sufficiently familiarized readers with various aspects of clinical depression, including symptoms, contemporary therapeutic approaches, and the need for mental health help. The road to recovery may be hard, but depression has many forms of help and effective interventions for better life quality. To know that content psychological assistance is the sign of strong characters, not weakness.
For whoever is suffering with those issues, it can be comforting to know that there is help out there. If you’re feeling very overwhelmed, think about calling a mental health professional right now. Alongside professional care, there are many online and community resources that can offer aid, information, and direction. Knowing what’s going on, getting timely help, and being part of a supportive community can help people regain some control over their own mental health.
Very Important Resources for Depression Help and Mental Health Support:
In the end, clinical depression is a complex medical condition requiring comprehensive assessment and treatment. These evaluations or treatments are for people just getting started or already up and down with depression; always know that help is available out there. Go to healthcare providers for a complete evaluation and to create that treatment plan tailored to individual needs. Because society seems to be growing up about how it views mental health, it is also now more important than ever to destigmatize depression and be receptive to effective treatments.
Finally, if you or someone you care for is in immediate danger or feeling suicidal, you must contact your local emergency services immediately. Your mental health matters, and a network of professionals and community resources is ready to help you. With proper early diagnosis, thorough treatment, and a supportive network, improved mental wellness can become a reality. Stay informed, seek help, and remember that recovery is possible.
As soon as you become aware of the symptoms and the tests for the diagnosis of depression, you can seek healing and well-being through the multitude of treatment options available to you. Knowledge is most vital in moving forward, while every positive step you take now will help walk out towards a brighter, healthier future.
So take note: every time you feel the signs of depression, reach out for mental health support and depression help. Your feelings are justified; help is available.
Test Test Test Test nnn112223333