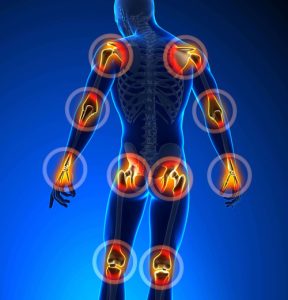
Joint pain is a health complaint from which millions of people across the globe suffer. It can develop in people of any age and when it’s there for some time can lead to drastic discomfort and a reduced quality of life. This resource is an extensive overspill on the causes, symptoms, diagnosis, treatment as well as prevention of joint pain. Backed by scientific research, evidence from acknowledged medical authorities, and clinical studies, this article acts as a great guide to understanding joint pain and management strategies. Whether your joints only pain occasionally or you are suffering from chronic joint pain, this guide is here to prepare you with all kinds of in-depth, reliable information and insights.
 Introduction
IntroductionJoint pain, or arthralgia as it is often called even in medical circles, may be caused by an acute injury or a chronic disease. Diagnosing the cause of joint pain is critical for its effective treatment given how complex this symptom can be. Joint pain can often be more than a fleeting discomfort, for instance, it may denote the existence of systemic or general diseases such as rheumatoid arthritis and osteoarthritis or even infection. Thus it is significant to recognize the biomechanics of joints, state their inflammatory processes, and identify one’s lifestyle factors when studying joint pain.
In this resource, we delve into:
Joint pain can arise from a multitude of underlying conditions. A proper diagnosis allows for treatment to be targeted exactly where it is needed. Some causes include the major ones such as listed below:
OA is one of the most common causes due to which older people deal with joint pain. Progressive degeneration of the cartilage cushion at the ends of bones occurs with age. This means that the bones will rub off each other and create pain, swelling, and reduction in movement. Clinical studies, including ones summarized by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), have proven that significant factors that enhance susceptibility include joint overuse, obesity, and hereditary predisposition.
Rheumatoid arthritis is an autoimmune disorder in which the immune system of the body mistakenly attacks the joint tissues. In this case, the joint lining undergoes inflammation, which causes a huge level of pain and damage to the tissues. Research published by the American College of Rheumatology further highlighted the insight into the chronic inflammatory process of rheumatoid arthritis, making early diagnosis and treatment important in order to avoid joint destruction.
Gout is a specific form of arthritis due to the deposition of uric acid crystals in joints. Therefore, acute episodes of gout in patients are characterized by intense pain, redness, and swelling. Dietary triggers include the ingestion of purine-rich foods (e.g., red meat, seafood) and alcohol. The mainstay of management incorporates lifestyle modifications and medications to lower urate levels.
Infectious arthritis is the term used to describe a situation when bacteria, viruses, or fungi invade and infect a joint. Bacterial arthritis is the most common type of arthritis and, if not treated brutally fast, may inflict lots of damage to the joint. The common bacteria responsible are Staphylococcus aureus and Streptococcus species. Prompt diagnosis is essential, as the rapid course of these infections may leave the only option for treatment being drainage and the administration of antibiotics.
Beyond rheumatoid arthritis, other autoimmune diseases such as lupus (systemic lupus erythematosus) may give rise to joint pain symptoms. In systemic lupus, the systemic inflammation is affecting multiple organs, including joints. A wealth of studies has been conducted supporting the use of immunosuppressive medications in aiding autoimmune-induced joint pain.
Joint injuries from accidents, falls, or sports-related incidents can present with acute joint pain. Any trauma may be spraining the ligaments, tearing the meniscus, or fracturing. Untreated injuries may evolve into chronic conditions over the years that predispose the affected individual to eventually suffer from osteoarthritis later in life.
Contingent factors such as obesity, a sedentary lifestyle, and poor biomechanical alignment may aggravate joint pain. Increased body weight augments the stress on joints like the knees and hips, contributing greatly to degenerative changes. Joint pain usually attributes to repetitive strain injuries and bad postures.
The symptoms of joint pain can differ widely based on the underlying cause. However, common signs and symptoms include:
Recognizing these symptoms is crucial in foreseeing the possible onset of joint problems. However, since many of these symptoms may overlap in different conditions, a thorough medical examination by a professional becomes paramount.
 Diagnosis
DiagnosisFor a proper diagnosis of joint pain, a complete evaluation of the patient’s history will be taken and a physical examination will be conducted, followed by a series of diagnostic tests. Here are the following entailments that may form the diagnostic procedures:
A medical professional will take a thorough medical history, including information about duration, severity, and pattern of the pain. The history also includes questions about previous injuries, family history of joint diseases, and any observable triggers. The physical examination assesses the tenderness, swelling, and motion of the joints, which helps narrow down the likely causes.
Imaging is of crucial importance in the diagnosis of joint disorders. Some of the most common imaging techniques include:
Many studies published in radiology journals show that imaging modalities have drastically improved the ability to diagnose joint conditions early and thus improve treatment outcomes.
Patients may undergo blood tests and fluid analyses to look for markers of inflammation, infection, or autoimmunity. Tests may include:
The information gained from laboratory tests is essential for distinguishing the forms of arthritis that exist, allowing proper direction of therapy.
The treatment of joint pain is generally complex and involves so many variables; types of patients presenting with different etiologies and symptomatology require different treatments. This interplay of diverse factors translates into treatment strategies that aim to minimize pain, restore function, and prevent additional joint harm. The following sections provide an overview of pharmacological whereas non-pharmacological treatment measures will follow thereafter.
The very first treatment option for relief of joint pain is medication. The type of medications includes:
Physical therapy has a vital place in joint pain treatment. Tailored exercise programs facilitate joint mobility, muscle strengthening around the joint, and overall reduction in discomfort. The common modalities include:
Research from rehabilitation and sports medicine advocates that adherence to an exercise program will reduce joint pain and even slow down the disease progression in degenerative joint diseases.
Some remedies are often used in conjunction with orthodox treatments for joint pain relief. These include:
For sudden debilitating joint pain that does not respond to conservative management, surgical options may come into play. These include:
The decision to operate is usually made on a per-patient basis, depending on the patient’s age, overall health status, and which joint is involved.
Although not all cases of joint pain can be prevented, lifestyle changes and immediate attention can drastically minimize risk factors and slow down the evolution of joint-related disorders.
Maintaining a healthy weight is crucial to reducing the load on weight-bearing joints like knees and hips. Studies prove that even a small percentage of weight loss can be associated with a significant reduction in joint pain and increase joint function. The weight management scheme comprises a balanced diet paired with exercise.
Regular exercise not only helps in weight maintenance but also helps with joint mobility and muscle strengthening. Low-impact activities such as swimming, cycling, and yoga may be particularly helpful for those at risk of developing joint pain. Consultation with a healthcare provider or physical therapist in creating a personal exercise plan is necessary.
The application of joint protection methods to everyday activities can minimize injury risk. Examples include the following:
The earlier you evaluate joint pains, the easier they are to manage. Being on the lookout for early signs of joint problems and seeking timely medical attention may keep minor problems from evolving into chronic problems. Regular consultations with your health care provider, especially among individuals with a family history of joint diseases, may lead to early diagnosis and intervention.
While joint inflammation is one of the first signs when something goes wrong, a wholesome load of omega-3 fatty acid-rich foods, as well as vitamin D and C, antioxidants, etc., indicate that these compounds might be useful in reducing the inflammatory process and improve function at the level of joints. Emerging evidence and literature are corroborating the role of nutrition in the management of inflammatory processes resulting from causes like arthritis and other joint disorders. Looking up the services of a nutrition advisor or dietitian can help when one wants to create a personal diet to address their needs.
The information provided herein is strongly backed with scientific evidence and clinical research. For instance, several longitudinal studies have signified the contribution of chronic inflammatory state in the pathogenesis of osteoarthritis and rheumatoid arthritis. The research published in esteem journals like The Journal of Rheumatology and Arthritis & Rheumatism dwelt much on the molecular drivers of joint degeneration, together with the efficacy of various treatment modalities.
Furthermore, recent trials have shown that patients suffering from joint pain exhibit beneficial outcomes as a result of a multimodal approach which integrates pharmacotherapeutic, physical therapy modalities, and lifestyle change. Medical bodies like the American College of Rheumatology are quasi-perpetual in continuously updating guidelines on recommendations to make them reflective of new evidence.
Joint pain cannot really be cured. It needs a lifestyle that would be preventive, and that involves taking measures more than just relieving pain. Some of the practical advice includes the following:
Joint pain manifests in various forms and it can significantly restrain its victim’s capacity to function in day-to-day life and, thus, his or her quality of life if not properly managed. By knowing various causes ranging from osteoarthritis and other degenerative diseases to autoimmune conditions like rheumatoid arthritis, and knowing the many symptoms, people will have better chances understanding the very complicated diagnoses and treatment techniques.
Management of joint pain through a concerted approach of combining the traditional medicine with specialized therapies, daily changes, and surgery when required. Indeed, the advances in medical science continue to add credence to what these authorities like NIAMS and the American College of Rheumatology recommend; they truly insist on early treatment and personalized treatment regimens.
Those who are considering options for treatment or looking forward to take preventive measures must certainly collaborate with healthcare providers. With the right-informed approach, many people with joint pain will stand to significant improvement, recover mobility, and thus great quality of life.
While this offers all the detail regarding joint pain and treatment, it is not intended as a replacement for a medical opinion. If symptoms persist or worsen over time, consult with a healthcare provider for an individualized evaluation and treatment plan.
For comprehensive and more insightful studies and exploration into these topics, try the following resources:
Being proactive and most importantly informed about joint health is the first step toward managing joint pain effectively. With the best mix of treatment and prevention, any person can lead an active, post-injury life despite suffering from joint pain.